Ayurveda (Sanskrit Āyurveda आयुर्वेद, “life–knowledge“; English pronunciation //[1]) or Ayurvedic medicine is a system of Hindu traditional medicine of Vedic tradition,[2] is native to the Indian subcontinent, and is a form of alternative medicine. The oldest known Ayurvedic texts are the Suśrutha Saṃhitā and the Charaka Saṃhitā. These Classical Sanskrit texts are among the foundational and formally compiled works of Ayurveda.
By the medieval period, Ayurvedic practitioners developed a number of medicinal preparations and surgical procedures for the treatment of various ailments.[3] Practices that are derived from Ayurvedic medicine are regarded as part of complementary and alternative medicine,[4] and along with Siddha Medicine and Traditional Chinese medicine, forms the basis for systems medicine.[5]
There is no scientific evidence for the effectiveness of Ayurvedic medicine for the treatment of any disease.[6] Concerns have been raised about Ayurvedic products; for example, peer-reviewed studies have shown that up to 20% of Ayurvedic U.S. and Indian-manufactured patent medicines sold through the internet contained toxic levels of heavy metals such as lead, mercury and arsenic.[7][8]
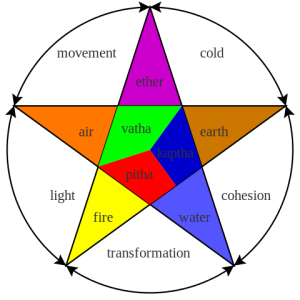
Much like the medicine of classical antiquity, Ayurveda has historically taken the approach of enumerating bodily substances in the framework of the five classical elements (Sanskrit [maha]panchabhuta, viz. earth, water, fire, air and ether. Moreover, Ayurveda names seven basic tissues (dhatu). They are plasma (rasa), blood (rakta), muscles (māmsa), fat (meda), bone (asthi), marrow (majja), and semen (shukra).[18]
Ayurveda states that a balance of the three elemental substances, the Doshas, equals health, while imbalance equals disease. There are three doshas: Vata, Pitta and Kapha. One Ayurvedic theory states that each human possesses a unique combination of these doshas which define this person’s temperament and characteristics. Each person has a natural state, or natural combination of these three elements, and should seek balance by modulating their behavior or environment. In this way they can increase or decrease the doshas they lack or have an abundance of them respectively. Another view present in the ancient literature states that dosha equality is identical to health, and that persons with imbalance of dosha are proportionately unhealthy, because they are not in their natural state of balance. Prakriti is one of the most important concepts in Ayurveda.
There are three principal early texts on Ayurveda, all dating to the early centuries of the Common Era. These are the Charaka Samhita, the Sushruta Samhita and the medical portions of the Bower Manuscript (also known as the Bheda Samhita). The relative chronology of these texts is not entirely clear. The Charaka Samhita is often cited as primary; although it survived only as a recension dating to the 4th or 5th century, it may be based on an original written between 100 BCE and 100 CE, in which case it would predate the other two texts. The Sushruta Samhita was written in the 3rd or 4th century. The Bower Manuscript is of particular interest because here the manuscript itself is ancient, dated to the early 6th century.[36] The earliest documented mention of the name Sushruta is found in the Bower Manuscript.[37] The medical portions of the Bower Manuscript constitutes a collection of recipes which are connected to numerous ancient authorities, and may be based on an older medical tradition practiced during the Maurya period, antedating both the Charaka and the Sushruta Samhitas.
The Bower Manuscript is also of special interest to historians due to the presence of Indian medicine and its concepts in Central Asian Buddhism. A. F. R. Hoernle in his 1897 edition identified the scribe of the medical portions of the manuscript as a native of India, using a northern variant of the Gupta script, who had migrated and become a Buddhist monk in a monastery in Kucha. The Chinese pilgrim Fa Hsien (c. 337–422 AD) wrote about the health care system of the Gupta empire (320–550) and described the institutional approach of Indian medicine, also visible in the works of Charaka, who mentions a clinic and how it should be equipped.[38]
Other early texts, sometimes mentioned alongside the Sushruta, Chakaka and Bheda texts, are the Kasyapa and the Harita samhitas, presumably dating to the later Gupta period (ca. 6th century). Ayurvedic authors of the 7th or 8th century include Vagbhata and Madhava.[39]
No significant scientific evidence has shown effectiveness of Ayurvedic medicine for the treatment of any disease, although massage and relaxation are often beneficial and there are indications of health effects from some herbal products used.[6] A systematic review of Ayurveda treatments for rheumatoid arthritis concluded that there was insufficient evidence, as most of the trials were not done properly, and the one high-quality trial showed no benefits.[73] A review of Ayurveda and cardiovascular disease concluded that the evidence for Ayurveda was not convincing, though some herbs seemed promising.[74]
Rasa shastra, the practice of adding metals, minerals or gems to herbs, may include toxic heavy metals such as lead, mercury and arsenic.[8] Adverse reactions to herbs due to their pharmacology are described in traditional Ayurvedic texts, but Ayurvedic practitioners are reluctant to admit that herbs could be toxic and that reliable information on herbal toxicity is not readily available; there is a communication gap between modern medicine practitioners and Ayurvedic practitioners.[76]
According to a 1990 study on Ayurvedic medicines in India, 41% of the products tested contained arsenic, and 64% contained lead and mercury.[48] A 2004 study found toxic levels of heavy metals in 20% of Ayurvedic preparations made in South Asia and sold in the Boston area; it concluded that Ayurvedic products posed serious health risks and should be tested for heavy-metal contamination.[77] A 2008 study of more than 230 products found that approximately 20% of remedies (and 40% of rasa shastra medicines) purchased over the Internet from U.S. and Indian suppliers contained lead, mercury or arsenic.[8][78][79] In 2012 the U.S. Centers for Disease Control and Prevention (CDC) linked Ayurvedic drugs to lead poisoning, based on some cases where toxic materials were found in the blood of pregnant women who had taken Ayurvedic drugs.[80]
Ayurvedic proponents believe that the toxicity of these materials is reduced through purification processes such as samskaras or shodhanas (for metals), similar to the Chinese pao zhi, although the Ayurvedic technique is more complex and may involve prayers as well as physical pharmacy techniques. However, these products have nonetheless caused severe lead poisoning and other toxic effects.[78][81]
Due to these concerns, the government of India ruled that Ayurvedic products must specify their metallic content directly on the labels of the product.[7] But, writing on the subject for Current Science, a publication of the Indian Academy of Sciences, M. S. Valiathan noted that “the absence of post-market surveillance and the paucity of test laboratory facilities [in India] make the quality control of Ayurvedic medicines exceedingly difficult at this time.”[7]
Most Ayurvedic products are labelled either for drug use (not FDA approved) or as dietary supplements. There is an import alert on some medicines issued by the FDA since 2007 which prevents these products entering the United States.[82]