Tag: obesity
Linoleic Acid in Soy Strongly Linked to the Obesity Epidemic
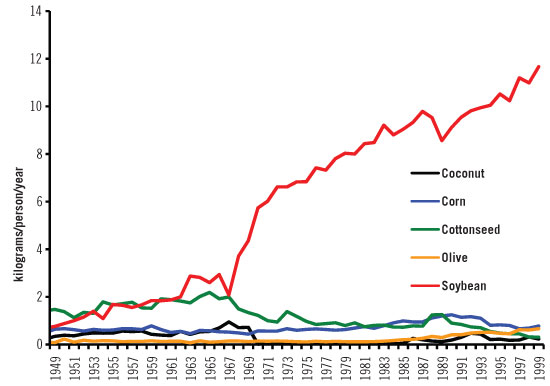
Soybean oil intake has increased dramatically for those eating the modern industrial food diet, and now research shows that this inexpensive oil contains high levels of a type of fat that’s contributing to the obesity epidemic.
Chart by National Institutes of Health
Can food really be as addictive as drugs?
Can Food Really Be Addictive? Yes, Says National Drug Expert
Compare the proportion of obese people in America to those who are addicted to drugs and then try to argue that food isn’t as addictive as crack cocaine, says Dr. Nora Volkow, the director of the National Institute on Drug Abuse.
Can food really be as addictive as drugs? In an impassioned lecture at Rockefeller University on Wednesday, Dr. Nora Volkow, director of the National Institute on Drug Abuse, made the case that the answer is yes and that understanding the commonalities between food and drug addictions could offer insights into all types of compulsive behavior.
Many of the neural signals involved in addictive behaviour also appear to be active in food reward. Naturally occurring opioids in the brain (including endorphins, enkephalins, dynorphins, and endomorphins) play an important role in neural reward processes that can lead to addictive behaviour. Both homeostatic and reward-based feeding mechanisms involve opioid peptide systems and opioid receptors, and opioid receptor blockers (antagonists) inhibit consumption of both addictive drugs and palatable food. Clinical trials targeting opioid receptors have revealed weight loss potential for opioid antagonists in obese patients. These relationships suggest the existence of a form of opioid-related addiction focused on palatable foods, although there are still major gaps in our knowledge of the molecular mechanisms through which opioids influence the hedonic properties of food.
Obesity rates in Korea are among the lowest in the OECD
Obesity rates in Korea are among the lowest in the OECD, but have been increasing steadily. About 4% of the adult population is obese in Korea, and about 30% are overweight (including obese). OECD projections indicate that overweight rates will increase by a further 5% within ten years.
obesity paradox
Fitness and fatness: not all obese people have the same prognosis
Second study sheds light on the ‘obesity paradox’
People can be obese but metabolically healthy and fit, with no greater risk of developing or dying from cardiovascular disease or cancer than normal weight people, according to the largest study ever to have investigated this, which is published online today (Wednesday) in the European Heart Journal [1].
The findings show there is a subset of obese people who are metabolically healthy – they don’t suffer from conditions such as insulin resistance, diabetes and high cholesterol or blood pressure – and who have a higher level of fitness, as measured by how well the heart and lungs perform, than other obese people. Being obese does not seem to have a detrimental effect on their health, and doctors should bear this in mind when considering what, if any, interventions are required, say the researchers.
Toward a Healthy Sustainable Food System
Date: Nov 06 2007Policy Number: 200712
Key Words: Climate Change, Food Security, Obesity, Occupational Health And Safety, Food
Purpose
In the United States, obesity and diet-related chronic disease rates are escalating, while the public’s health is further threatened by rising antibiotic resistance; chemicals and pathogens contaminating our food, air, soil and water; depletion of natural resources; and climate change. These threats have enormous human, social, and economic costs that are growing, cumulative, and unequally distributed. These issues are all related to food—what we eat and how it is produced. The US industrial food system provides plentiful, relatively inexpensive food, but much of it is unhealthy, and the system is not sustainable. Although most US food consumption occurs within this industrial system, healthier and more sustainable alternatives are increasingly available.
The American Public Health Association (APHA) has long been active on food system issues, as is shown by the large body of relevant policy. Moving toward a healthier and more sustainable food system will involve tackling longstanding challenges and addressing new and evolving demands. This position paper reviews the scientific basis for understanding the US food system and sustainability, identifies specific issues of concern, discusses key related policies and action opportunities, and outlines APHA goals. By uniting multiple food system themes in a single statement, it aims to provide clarity, new emphases, and solid direction, encouraging the APHA to increase its activities and leadership to promote a more sustainable, healthier, and more equitable food system.
Diabetes is not a disease; it is a reaction of the body to survive
A body does not want to die. Nobody just likes to die, to give up, and kick the bucket. Physical discomfort is another story.
Diseases, or, that what we describe as disease are always the result of ‘something’. Colds can be sustained by coldness and rain. A broken leg can be caused by a fall. If you do not eat, you feel hungry.
You get appetite due to an empty stomach. If we eat food, the feeling will disappear. Then food was the right solution. This is not a disease, but a question of too little food.
Diabetes, a word often heard today, and it is used often, as it comes in handy. Was diabetes in earlier times also a term en vogue? Even small children are confronted with this diagnose; is this normal?
Diabetes and obesity often go together.
Our bodies however have to accept anything we eat. We use, for example, unhealthy spreads on our sandwich; spreads, only ‘one molecule different from plastic’.
The Fast Metabolism Diet
Haylie Pomroy has helped countless clients lose up to 20 pounds in just 4 weeks –all through the fat-burning power of food. Hailed as “the metabolism whisperer,” Haylie reminds us that food is not the enemy, it’s the rehab needed to rev-up your sluggish, broken-down metabolism and turn your body into a fat-burning furnace.
On this plan you’re going to eat a lot. You’re going to eat three full meals and at least two snacks a day – and you’re still going to lose weight. What you’re not going to do is count a single calorie or fat gram. You’re going not to ban entire food groups. You’re not going to go carb-free or vegan or go cold turkey on the foods you love. Instead, you’re going to rotate what you’re eating throughout each week according to a simple and proven plan carefully designed to induce precise physiological changes that will set your metabolism on fire.
Phase I (Monday-Tuesday): Lots of carbs and fruits
Phase II (Wednesday-Thursday): Lots of proteins and veggies
Phase III (Friday-Sunday): All of the above, plus healthy fats and oils
Continue reading “The Fast Metabolism Diet”
What has your food been eating?
What has your food been eating?
Laurent Adamowicz at TEDxBeaconStreet
Published on Mar 18, 2013
Having seen the very best, the worst, and the ugliest of the food industry, Laurent Adamowicz gives a poignant account of how our food system has dramatically changed over the last two decades. Could the obesity epidemic be directly linked to what our food has been eating?
Senior Fellow 2011 in the Advanced Leadership Initiative at Harvard University, Laurent Adamowicz is a former food industry executive and serial entrepreneur. He is the founder & CEO of Bon’App, a simple nutrition guidance mobile application that tells you what’s in your food.
In the spirit of ideas worth spreading, TEDx is a program of local, self-organized events that bring people together to share a TED-like experience. At a TEDx event, TEDTalks video and live speakers combine to spark deep discussion and connection in a small group. These local, self-organized events are branded TEDx, where x = independently organized TED event. The TED Conference provides general guidance for the TEDx program, but individual TEDx events are self-organized.* (*Subject to certain rules and regulations)
Hepatitis
Hepatitis (plural: hepatitides) is a medical condition defined by the inflammation of the liver and characterized by the presence of inflammatory cells in the tissue of the organ. Hepatitis may occur with limited or no symptoms, but often leads to jaundice, poor appetite and malaise. Hepatitis is acute when it lasts less than six months and chronic when it persists longer. The condition can be self-limiting (healing on its own) or can progress to fibrosis (scarring) and cirrhosis.
Worldwide, causes include autoimmune diseases and ingestion of toxic substances (notably alcohol, certain medications, some industrial organic solvents, and plants).
Viral hepatitis is the most common cause of hepatitis worldwide.[5] Other common causes of non-viral hepatitis include toxic and drug-induced, alcoholic, autoimmune, fatty liver, and metabolic disorders.[6] Less commonly some bacterial, parasitic, fungal, mycobacterial and protozoal infections can cause hepatitis.[7][8] Additionally, certain complications of pregnancy and decreased blood flow to the liver can induce hepatitis.[7][9] Cholestasis (obstruction of bile flow) due to hepatocellular dysfunction, biliary tract obstruction, or biliary atresia can result in liver damage and hepatitis.[10][11]
The term is derived from the Greek hêpar (ἧπαρ), meaning “liver,” and the suffix -itis (-ῖτις), meaning “inflammation” (c. 1727).[2]
Non-alcoholic fatty liver disease (NAFLD) is one cause of a fatty liver, occurring when fat is deposited (steatosis) in the liver not due to excessive alcohol use. It is related to insulin resistance and the metabolic syndrome and may respond to treatments originally developed for other insulin-resistant states (e.g. diabetes mellitus type 2) such as weight loss, metformin and thiazolidinediones.[1] Non-alcoholic steatohepatitis (NASH) is the most extreme form of NAFLD, and is regarded as a major cause of cirrhosis of the liver of unknown cause.[2]
Most patients with NAFLD have few or no symptoms. Patients may complain of fatigue, malaise, and dull right-upper-quadrant abdominal discomfort. Mild jaundice may be noticed although this is rare. More commonly NAFLD is diagnosed following abnormal liver function tests during routine blood tests. By definition, alcohol consumption of over 20 g/day (about 25 ml/day of net ethanol) excludes the condition.[1]
NAFLD is associated with insulin resistance and metabolic syndrome (obesity, combined hyperlipidemia, diabetes mellitus (type II) and high blood pressure).[1][2]
Common findings are elevated liver enzymes and a liver ultrasound showing steatosis. An ultrasound may also be used to exclude gallstone problems (cholelithiasis). A liver biopsy(tissue examination) is the only test widely accepted as definitively distinguishing NASH from other forms of liver disease and can be used to assess the severity of the inflammationand resultant fibrosis.[1]
Non-invasive diagnostic tests have been developed, such as FibroTest, that estimates liver fibrosis,[7] and SteatoTest, that estimates steatosis,[8] however their use has not been widely adopted.[9] Apoptosis has been indicated as a potential mechanism of hepatocyte injury as caspase-cleaved cytokeratin 18 (M30-Apoptosense ELISA) in serum/plasma is often elevated in patients with NASH; however, as the role of oncotic necrosis has yet to be examined it is unknown to what degree apoptosis acts as the predominant form of injury.[10][11]
Other diagnostic tests are available. Relevant blood tests include erythrocyte sedimentation rate, glucose, albumin, and renal function. Because the liver is important for making proteins used in coagulation some coagulation related studies are often carried out especially the INR (international normalized ratio). Blood tests (serology) are usually used to rule out viral hepatitis (hepatitis A, B, C and herpes viruses like EBV or CMV), rubella, and autoimmune related diseases. Hypothyroidism is more prevalent in NASH patients which would be detected by determining the TSH.[12]
It has been suggested that in cases involving overweight patients whose blood tests do not improve on losing weight and exercising that a further search of other underlying causes be undertaken. This would also apply to those with fatty liver who are very young or not overweight or insulin-resistant. In addition those whose physical appearance indicates the possibility of a congenital syndrome, have a family history of liver disease, have abnormalities in other organs, and those that present with moderate to advanced fibrosis or cirrhosis.[13]
Management
A large number of treatments for NAFLD have been studied. While many appear to improve biochemical markers such as alanine transaminase levels, most have not been shown to reverse histological abnormalities or reduce clinical endpoints:[1]
- Treatment of nutrition and excessive body weight:
- Nutritional counseling: Diet changes have shown significant histological improvement.[14] Specifically, avoiding food containing high-fructose corn syrup and trans-fats is recommended.[15]
- Weight loss: gradual weight loss may improve the process in obese patients; rapid loss may worsen NAFLD. Specifically, walking or some form of aerobic exercise at least 30–45 minutes daily is recommended.[15] The negative effects of rapid weight loss are controversial: the results of a meta-analysis showed that the risk of progression is very low.[16]
- A recent meta-analysis presented at the Annual Meeting of the American Association for the Study of Liver Diseases (AASLD) reported that weight-loss surgery leads to improvement and or resolution of NASH in around 80% of patients.[17]
- Insulin sensitisers (metformin[18] and thiazolidinediones[19]) have shown efficacy in some studies.
- ursodeoxycholic acid and lipid-lowering drugs, have little benefit.[citation needed]
- Vitamin E: Vitamin E can improve some symptoms of NASH and was superior to insulin sensitizer in one large study. In the Pioglitazone versus Vitamin E versus Placebo for the Treatment of Nondiabetic Patients with Nonalcoholic Steatohepatitis (PIVENS) trial, for patients with NASH but without diabetes mellitus, the use of very high dosages of vitamin E (800 IU/day) for four years was associated with a significantly higher rate of improvement than placebo (43% vs. 19%) in the primary outcome. The primary outcome was an improvement in certain histological features as measured by biopsy—but it did not improve fibrosis. Pioglitazone, an insulin sensitizer, improved some features of NASH but not the primary outcome, and resulted in a significant weight gain (mean 4.7 kilograms) which persisted after pioglitazone was discontinued.[20]
- Statin: Improvements in liver biochemistry and histology in patients with NAFLD through treatment with statins have been observed in numerous cases, although these studies were carried out on a relatively small sample of patients.[21] Statins have also been recommended for use in treating dyslipidemia for patients with NAFLD.
- Modest wine drinking: In a study using the NHANES III dataset, it has been shown that mild alcohol consumption (one glass of wine a day) reduces the risk of NAFLD by half.[22]
Epidemiology
The prevalence of non-alcoholic fatty liver disease ranges from 9 to 36.9% of the population in different parts of the world.[23][24][25] Approximately 20% of the United States population suffers from non-alcoholic fatty liver, and the prevalence of this condition is increasing.[26] The prevalence of non-alcoholic fatty liver disease is higher in Hispanics, which can be attributed to high rates of obesity and type 2 diabetes in Hispanic populations.[27] Non-alcoholic fatty liver disease is also more common among men than women in all age groups until age 60, where the prevalence between sex equalize. This is due to the protective nature of estrogen.[28]